Kratom — Herbal Medicine, Drug, or Both?
Part 2 of Series: Natural, But Not Neutral
(Educational only — not medical advice.)
Kratom — Herbal Medicine, Drug, or Both?
Educational only; not medical advice. If you have symptoms, are pregnant, or take medications, consult a licensed clinician.
Kratom is a botanical that forces a hard conversation: you can buy it like a supplement and talk about it like an herbal remedy, but its effects can be drug-like and its risks can be serious. That makes “Is it a drug or medicine?” a real question—not a semantic one.
Sources: NIDA (NIH): Kratom | FDA: FDA and Kratom | Mayo Clinic: Kratom — Unsafe and Ineffective | CDC Archive: Salmonella infections linked to kratom (2018) — Final Update
What it is and why the conversation is polarized
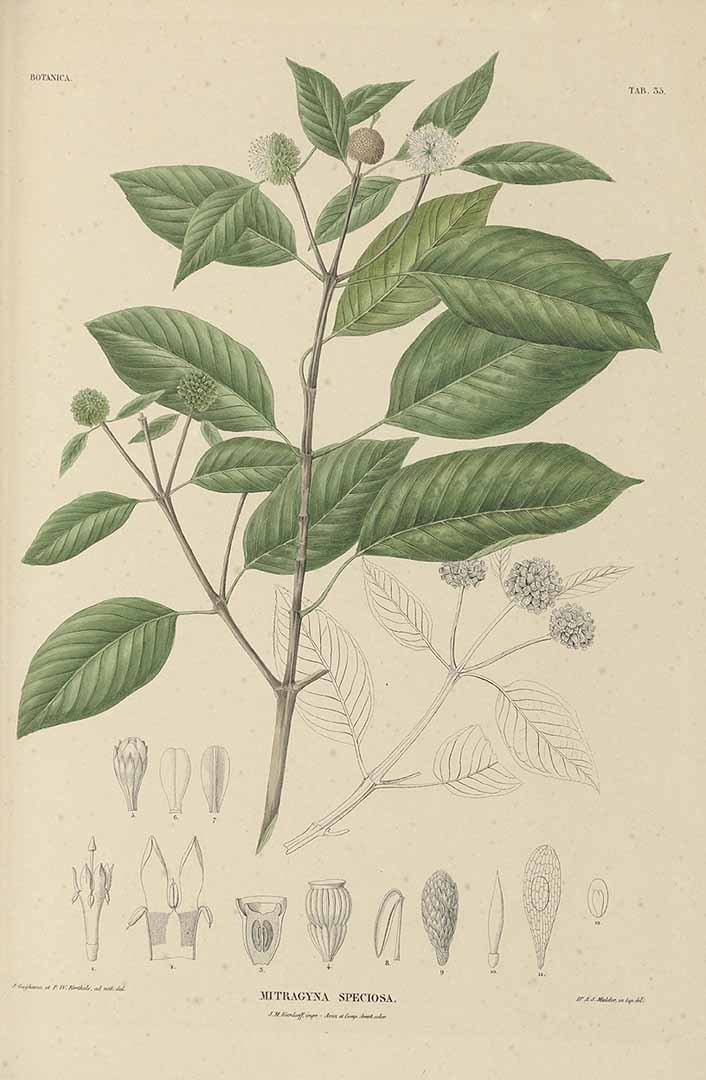
Kratom (Mitragyna speciosa) is a tree native to Southeast Asia. Its leaves contain alkaloids that can produce stimulant-like effects in some contexts and opioid-like effects in others—one reason the public conversation swings between “helpful plant” and “dangerous drug.”
In the U.S., kratom is sold in powders, capsules, and concentrated extracts. This variation in product form is central: potency can differ dramatically between plain leaf products and high-potency extracts.
Sources: NIDA: Kratom overview | FDA: FDA and Kratom
Drug vs. medicine vs. supplement: the clean framing
Is it a drug? Pharmacologically, kratom can behave like one, and federal agencies describe risks in drug-like terms (including dependence, withdrawal, and serious adverse events). FDA also states there are no FDA-approved kratom drug products legally on the market in the U.S.
Is it medicine? Historically, kratom has been used traditionally, and many U.S. users report taking it to self-manage pain or opioid withdrawal. But kratom is not an FDA-approved treatment for pain, anxiety, or opioid use disorder, and “used as medicine” does not equal “proven medicine.”
Is it a supplement? Many sellers market it in supplement-like ways, but FDA has repeatedly warned consumers not to use kratom and has taken actions related to illegal marketing. That tension—retail availability vs. strong federal warnings—is exactly why kratom belongs in this series.
Sources: FDA: FDA and Kratom | NIDA: Kratom overview | Mayo Clinic: Kratom overview
What people say online (and why it’s not evidence)
Online discussions often describe kratom as (1) a mood/energy booster, (2) a pain reliever, and (3) a bridge away from opioids. These accounts can be sincere, but they are not controlled evidence. They also don’t control for potency, co-use with other substances, or placebo/nocebo effects.
For a general-audience blog, it’s reasonable to acknowledge lived experience while still stating the high-stakes reality: self-treatment for pain or withdrawal is medically complex and can be risky without supervision.
Sources: NIDA: Kratom overview | Mayo Clinic: Kratom — unsafe and ineffective
Safety and quality risks that aren’t theoretical
FDA warnings cite serious adverse events including liver toxicity, seizures, and substance use disorder. FDA also notes that deaths where kratom was present often involved other substances (making the role of kratom hard to isolate, but the risk still meaningful).
On the quality side, contamination is a documented hazard. The CDC investigated a multistate Salmonella outbreak linked to kratom products and warned that contaminated kratom could continue to cause illness because no single common source was identified.
A newer layer of concern is the emergence of concentrated kratom-related derivatives such as 7-hydroxymitragynine (7-OH). FDA has issued communications targeting certain 7-OH products due to opioid-receptor activity and abuse potential, emphasizing that these products are distinct from natural leaf products.
Sources: FDA: FDA and Kratom | CDC: Salmonella outbreak linked to kratom (final update) | FDA: Steps to restrict 7-OH opioid products
A responsible reader takeaway (harm reduction framing, not how-to)
If someone is considering kratom, the responsible message is not “how to use it,” but “how to evaluate risk.”
1) Treat kratom as a bioactive substance with dependence potential. If use becomes daily, escalating, or “needed to feel normal,” that’s a warning sign.
2) Avoid mixing with other sedating substances (alcohol, opioids, benzodiazepines, sleep meds) without medical oversight; stacking depressants increases danger.
3) Be especially cautious with extracts and high-potency products; they can shift risk quickly.
4) If the goal is opioid withdrawal support or chronic pain management, consider medical alternatives and supervision.
Sources: FDA: FDA and Kratom | NIDA: Kratom overview
Short FAQ (blog-friendly)
Is kratom federally approved as medicine? No. There are no FDA-approved kratom drug products legally marketed in the U.S.
Is kratom “a drug”? It can have drug-like effects, and public health agencies describe risks that include dependence and serious adverse events.
Why do opinions differ so much? Experiences vary with product potency, co-use with other substances, and individual biology—and the marketplace includes everything from leaf powder to concentrated derivatives.
Sources: FDA: FDA and Kratom | NIDA: Kratom overview
References
Mayo Clinic: Kratom — Unsafe and Ineffective
CDC Archive: Salmonella infections linked to kratom (2018) — Final Update
CDC Archive: Advice to Consumers — Kratom and Salmonella
FDA Press Announcement: FDA Takes Steps to Restrict 7-OH Opioid Products
Series promise: “We separate tradition, internet claims, science, and regulation—so you can decide what belongs in your wellness routine.”