Ashwagandha — Supplement, Medicine, or a Drug-Like Herb?
Part 1 of Series: Natural, But Not Neutral
(Educational only — not medical advice.)
Ashwagandha is one of the most popular “stress support” botanicals in the U.S., and it sparks a persistent argument: is it a drug, is it medicine, or is it “just a supplement”? The honest answer is that it can be discussed as all three—depending on whether you mean the legal definition of a drug, the cultural meaning of medicine, or the regulatory category it’s sold under.
Sources: NCCIH: Ashwagandha — Usefulness and Safety | NIH ODS: Ashwagandha — Health Professional Fact Sheet | NIH ODS: Ashwagandha — Consumer Fact Sheet | FDA: Structure/Function Claims for Dietary Supplements
What it is and how it’s sold
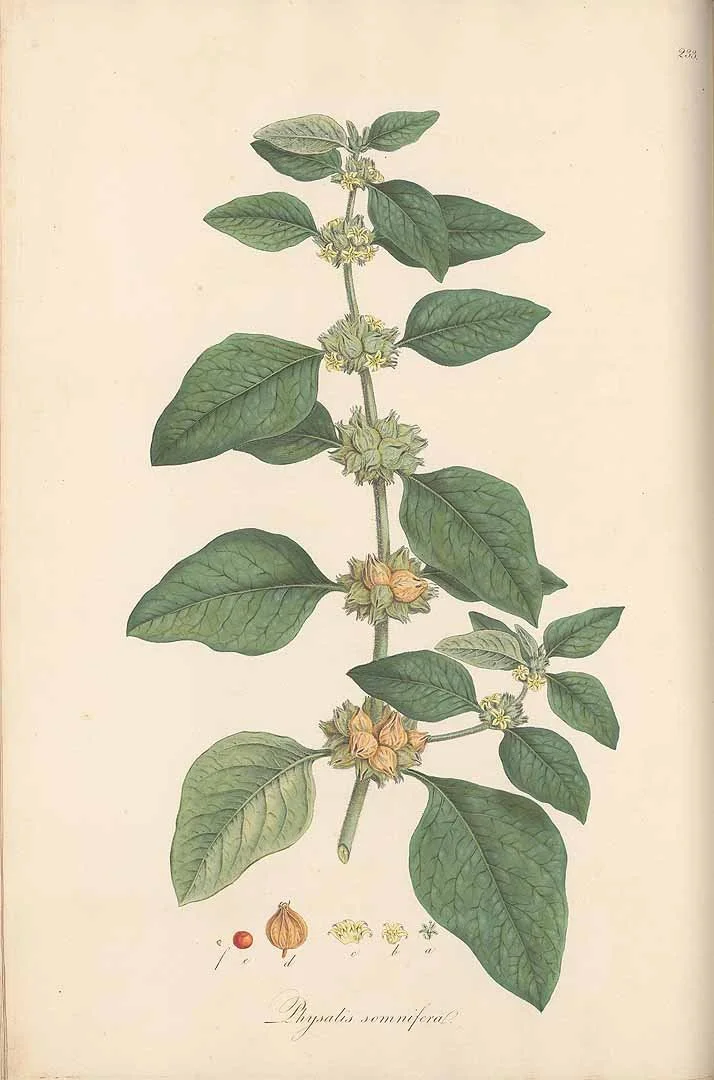
Ashwagandha (Withania somnifera) is an herb used for centuries in Ayurvedic traditions. In modern retail, it’s most commonly sold as capsules, powders, teas, and standardized extracts. That “extract” detail matters: different products can contain different plant parts (root vs. leaf), different extraction methods, and different levels of bioactive compounds—so consumers often compare experiences that aren’t truly comparable.
In the U.S., ashwagandha is generally marketed as a dietary supplement, which means it does not go through the same premarket approval process required for prescription drugs. Instead, companies are responsible for ensuring their product is safe and properly labeled, and regulators typically step in after problems are identified.
Sources: NCCIH: Ashwagandha (usefulness & safety) | FDA: Dietary supplements Q&A | ODS: Ashwagandha (health professional)
The core question: drug vs. medicine vs. supplement
If you mean “drug” in the legal/regulatory sense, most ashwagandha products in the U.S. are not drugs—they’re supplements. A practical rule of thumb: products that claim to diagnose, treat, cure, or prevent disease are making drug-type claims. Supplement labels typically avoid that language and instead use “structure/function” wording like “supports stress response,” which is allowed when paired with the required disclaimer.
If you mean “medicine” in the broader, cultural sense—something people use therapeutically—ashwagandha is used as medicine in traditional contexts and in modern wellness routines. The tension is that “used as medicine” doesn’t automatically mean “proven as medicine” under clinical standards.
Sources: FDA: Structure/function claims | ODS: Ashwagandha (consumer) | NCCIH: Ashwagandha (usefulness & safety)
What the evidence supports (and what it doesn’t)
Most of the serious interest in ashwagandha revolves around stress, anxiety, and sleep. Federal health resources summarize multiple studies suggesting ashwagandha may reduce stress and anxiety and may improve sleep, but they also emphasize that studies use different extracts and doses and that additional research is needed for confident conclusions.
That variability is not a minor technicality—it is the main reason supplement conversations become confusing. A person may say, “It worked for me,” and they may be correct for the specific extract and dose they used, while another person using a different formulation sees no effect.
A responsible consumer summary is: there’s a plausible short-term signal for stress and sleep, but the evidence isn’t strong enough to treat it as a dependable, standardized medical therapy—especially for severe symptoms or complex medical conditions.
Sources: ODS: Ashwagandha (consumer) | ODS: Ashwagandha (health professional) | NCCIH: Ashwagandha (usefulness & safety)
Safety: where “natural” stops being a comfort word
Online, ashwagandha is often framed as gentle. In reality, it’s bioactive, and bioactive substances have tradeoffs. Commonly reported side effects include drowsiness and gastrointestinal upset.
The bigger safety topic is rare but serious: there are published reports linking ashwagandha supplements to liver injury. This appears to be uncommon, but it’s a reminder that supplements can produce medically significant harm, particularly in vulnerable individuals or with certain product-quality issues.
Sources: NCCIH: Ashwagandha (usefulness & safety) | LiverTox: Ashwagandha
Practical consumer checklist (without pretending it’s harmless)
1) Treat ashwagandha like an active product, not a “vitamin.” Avoid stacking it with other sedating products unless a clinician approves.
2) Prioritize quality signals: third-party testing, clear labeling (root vs. leaf, standardized extract), and reputable manufacturing practices.
3) If you are pregnant, have liver disease, have thyroid concerns, or take prescription medications—especially sedatives or medications with narrow therapeutic windows—consult a clinician or pharmacist before using it.
4) Stop and seek medical advice if you develop symptoms suggestive of liver problems (for example, jaundice or dark urine).
Sources: NCCIH: Ashwagandha (usefulness & safety) | ODS: Ashwagandha (health professional) | LiverTox: Ashwagandha
Short FAQ
Is ashwagandha a prescription medication? No—most products are sold as dietary supplements in the U.S.
Is it “medicine”? In traditional systems and in common language, many people use it that way. Clinically, it has emerging evidence for stress/sleep but isn’t a standardized, FDA-approved therapy.
Can it interact with medications? Potentially. If you take medications or have ongoing conditions, check with a clinician or pharmacist before starting.
Sources: FDA: Dietary supplements Q&A | NCCIH: Ashwagandha
References
NCCIH: Ashwagandha — Usefulness and Safety
NIH ODS: Ashwagandha — Health Professional Fact Sheet
NIH ODS: Ashwagandha — Consumer Fact Sheet
FDA: Structure/Function Claims for Dietary Supplements
Series promise: “We separate tradition, internet claims, science, and regulation—so you can decide what belongs in your wellness routine.”